ACL Tear, Repair & Revision
A board-certified, fellowship-trained orthopaedic knee surgeon and sports medicine specialist, Dr. Steven Chudik is renowned for his arthroscopic knee expertise and innovative procedures that reduce surgical trauma, speed recovery and yield excellent outcomes.
Through his research, Dr. Chudik investigates and pioneers advanced and novel arthroscopic procedures, instruments and implants that have forever changed patients’ lives. Never content to settle for what’s always been done for orthopaedic knee care, Dr. Chudik prides himself on providing individualized care and developing a plan that is right for each patient. By taking this approach for the past 20 years, Dr. Chudik has developed minimally invasive surgical techniques, instruments and implants for the arthroscopic repair, reconstruction and revision-reconstruction of anterior cruciate ligament (ACL) injuries, pediatric growth plate-sparing ACL surgery, and meniscus repair, as well as injury-specific rehabilitation programs and return to sport protocols and testing.
ACL Expertise
- Arthroscopic anatomic ACL reconstruction
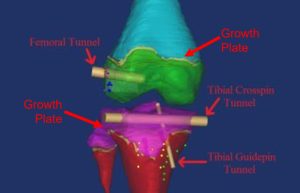
- Arthroscopic physeal-sparing (growth plate) reconstruction in skeletally immature pediatric patients (Developed by Dr. Chudik)
- Complex arthroscopic revision surgery for previously failed ACL reconstructions
- Arthroscopic Tibial Spine Avulsion Surgery for Pediatric Patients
- Anterolateral ligament reconstruction
- Tunnelless ligament reconstruction (Under development by Dr. Chudik)
- Arthroscopic meniscus repair
- Arthroscopic meniscectomy
- Arthroscopic partial meniscectomy
- Arthroscopic meniscal root repair
- Arthroscopic meniscus transplant
- Return to sport Neuromuscular training program
- Return to sport testing
Individualized Treatment and Rehabilitation
Because no two people and no two injuries are alike, Dr. Chudik uses his expertise to develop and provide individualized care and recovery plans for his patients. This customized attention explains why patients travel to have Dr. Chudik care for their knee injuries, especially pediatric ACL injuries and patients with failed ACL surgeries.
To ensure his ACL patients can return to sports and activities safely, Dr. Chudik researched and developed a return to sport functional test protocol that provides objective measures for both the athlete and Dr. Chudik to know when it is safe to return, as well as what else needs to be done if the athlete fails to pass the exam.
Frequently Asked Questions
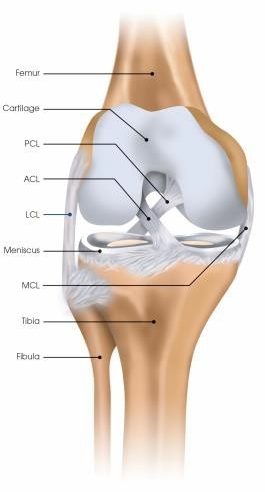
The anterior cruciate ligament (ACL) is one of four main rope-like structures that stabilize the knee joint by connecting the femur (thigh bone) to the tibia and fibula (leg bones). The ACL specifically prevents anterior translation (forward movement) and internal rotation of the tibia relative to the femur. The ACL stabilizes the knee during planting, jumping, landing, stopping, cutting, and pivoting maneuvers. The ACL is one of the most commonly injured structures of the knee in young competitive athletes.
The ACL is most often torn by a non-contact mechanism when an athlete attempts to plant, jump, land, stop, cut, or pivot on a single leg. Contact injuries can also occur when the knee sustains a direct blow, but this is less common. ACL injuries also occur during skiing with possibly a different mechanism.
When an athlete tears their ACL, they often perceive a “pop” while planting on a single leg during an athletic maneuver. The degree of initial pain is variable but most athletes are unable to continue playing. Swelling is often delayed but typically occurs within hours of the injury. Swelling and pain often make it difficult to walk after the initial injury. Returning to play following the injury risks further injury to the meniscus, cartilage, and other structures. Without surgery, patients often experience continued episodes of instability and giving way.
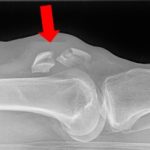
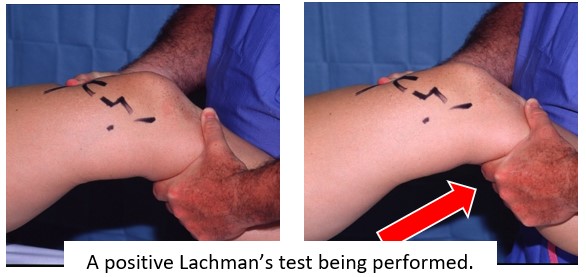
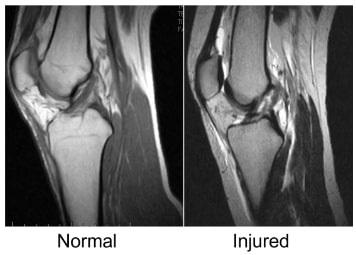
An ACL tear is diagnosed with a combination of patient history of the mechanism of injury and physical exam. X-rays and Magnetic Resonance Imaging (MRI) help confirm an ACL tear and determine if there are other associated injuries including fractures and other ligament, meniscal or cartilage tears. Most often, the history involves a younger competitive athlete (females more common than males) who report injuring their knee. They are usually unable to continue playing and experience pain, swelling, and difficulty bearing weight. On physical exam, Dr. Chudik will check for the presence of an effusion (swelling in the knee), loss of knee range of motion, inability of the quadriceps to properly contract, and perform a ligament exam including a Lachman exam. The Lachman exam specifically tests the function of the ACL and is positive when the tibia is able to be pulled forward relative to the femur without a perceptible endpoint provided by an intact ACL.
An MRI is ordered which confirms the suspected ACL tear and reveals the extent of tearing and possible injury to other surrounding structures.

The majority of ACL tears are functionally complete which prevents athletes, even recreational ones, from returning to athletic activities due to knee instability and giving way. Additionally, attempting to return to activities without an ACL risks further injury to the meniscus and cartilage of the knee with any single instability episode. Living without an ACL places increased stress on the meniscus of the knee and can lead to break down and tears of the meniscus without returning to risky sport activities. Therefore, most patients choose to have surgery to reconstruct their ACL. Pediatric patients with open growth plates sometimes require surgery that avoids injury to their growth plate as non-operative treatment has been shown to result in continued instability, meniscus tears, and further damage to the knee.
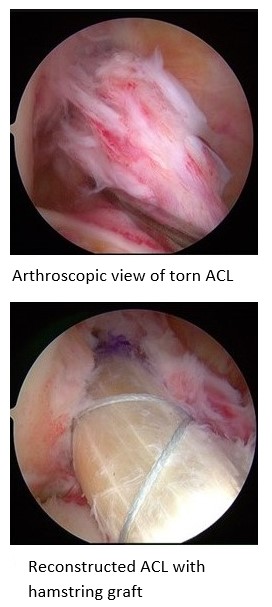
Surgery to repair the ACL is not as reliable reconstructing (replacing) the ACL using a tendon graft. There are several autologous (from the patient) graft options including bone-patellar tendon-bone, hamstring, quadriceps, and iliotibial band. Dr. Chudik prefers not to use allogenic tendon graft (allografts) from cadavers which have been shown to result in higher rates of re-tear. Surgery can be performed after the swelling and range of motion are restored for the injured knee which generally requires 2 to 3 weeks of physical therapy following the injury. During ACL surgery, the torn ligament is reconstructed (replaced) with a tendon graft because the ligament is damaged such that a simple repair is often not successful. The goals of the surgery are to reconstruct the torn ligament, repair any other damaged structures (including other ligaments, the meniscus, and cartilage) and restore function and stability to the knee.
- The surgery is typically performed as an outpatient procedure (patient goes home the same day after surgery) with lighter general anesthesia and an adductor and possibly an IPACK nerve block to numb the knee.
- A patient can expect to be on crutches and partial weight bearing for approximately 4 weeks following an isolated ACL reconstruction to protect the graft.
- A post-op knee brace is worn for only 24 hours to ambulate while the nerve block is working and used to help keep the knee straight at night while sleeping.
- If the meniscus is also repaired during surgery, the patient will use crutches and wear a brace locked in full extension (straight) for 6 weeks.
- The brace may also be needed if other ligaments required surgery as well but this is typically known from the MRI.
- Following surgery, the incisions should be kept clean and dry for the first 14 days after surgery. Showering lightly is allowed after 2 weeks but wounds cannot be submerged underwater for at least 3 weeks after surgery.
- A patient may drive after 6 weeks if the driving right lower extremity is involved.
- Home exercises focusing on straightening the knee and contracting the quadriceps muscles begin immediately in the recovery room and are performed on an hourly basis.
- Physical therapy begins days after surgery and will be required to restore motion, strength, and proprioception (balance) following reconstruction.
- Strengthening, biking, and range of motion exercises are emphasized and prolonged walking and standing are discouraged during the first three months following surgery.
- Prolonged immobilization associated with sitting, driving, and flying are avoided for the first six weeks following surgery to prevent deep vein thrombosis (DVT)(clot) formation.
- Recovery varies from 6 to 12 months depending on the injury and the patient.
A patient may return to school or sedentary work in just less than 1 week if the patient can use crutches, elevate the extremity, perform their exercises frequently, and get up and move around regularly to avoid deep vein thrombus (DVT) (clot) formation.
After the knee is fully rehabilitated and physical therapy is completed, Dr. Chudik recommends competitive athletes participate in a 6 week return to sport training program and also pass Dr. Chudik’s ACL Return to Sport Test to ensure the athlete is safe to return to sport. The test is performed to confirm that the knee is fully rehabilitated and more importantly, to confirm that errors in movement patterns known to put patients at risk for re-injury are corrected. Timelines for return to sport vary depending on the patient, the extent of the injury, and the sport. A full return to sports participation can take anywhere from 6 to 12 months.
ACL reconstructed knees generally perform well over our athletic lifetime, especially when maintained with an appropriate regimen of strength training, flexibility, and activity. More importantly, non-impact activities such as biking, or water sports usually provide optimal fitness to the knee without overdoing it. It is important to remember that any bone or joint with a history of injury such as an ACL tear is more susceptible to an early onset of arthritis.
Testimonials and Patient Stories
Knee Anatomy
Your knees are the most commonly injured joints in your body. Unlike your shoulder that moves in all directions, your knees appear only to bend and straighten, but actually their movements are much more complex and involve rotation, translation, sliding and rolling.
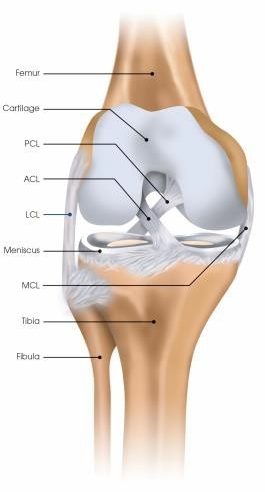
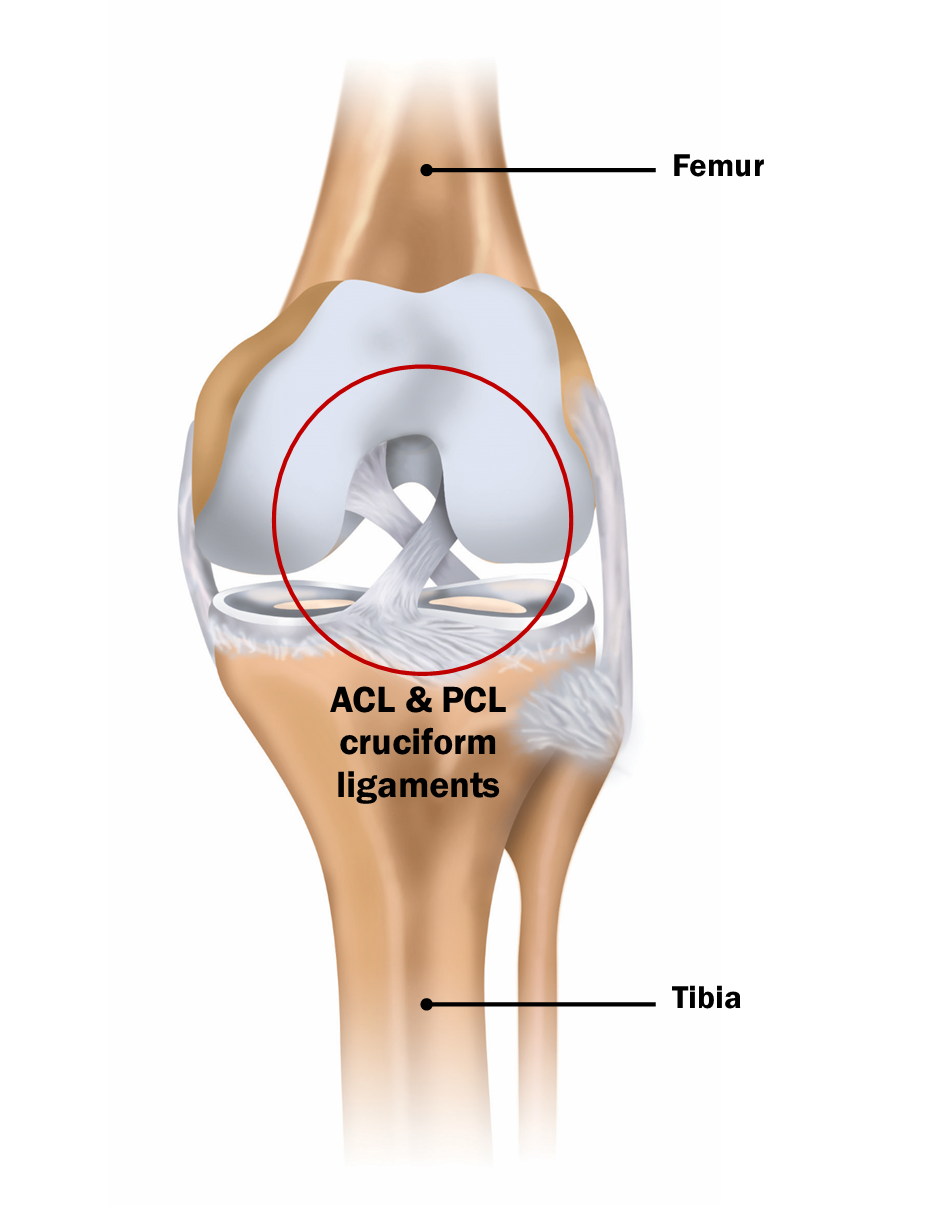
Ligaments
There are five main ligaments connecting the bones at the knee joint and provide stability when you walk, run and jump. They are the:
- Anterior cruciate ligament (ACL)
- Posterior cruciate ligament (PCL)
- Medial collateral ligament (MCL)
- Posterolateral corner (PLC) ligaments including the lateral collateral ligament (LCL)
- Anterolateral ligament (ALL)
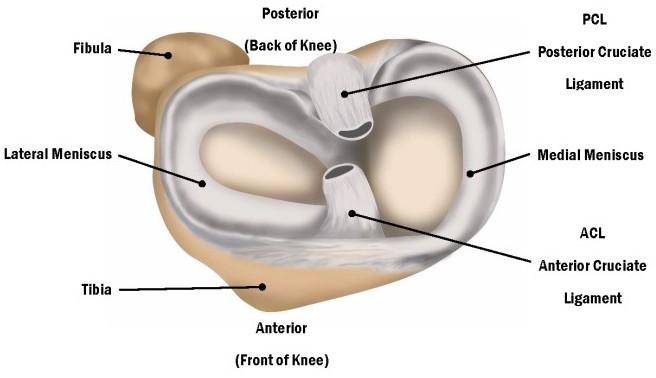
Cartilage and Meniscus
The joint surface of the knee is covered with a thin, but durable layer of cartilage over the ends of the femur, tibia, and patella and, along with the meniscus, allows the knee surfaces to articulate, move smoothly—almost frictionless and painlessly along each other. The cartilage lacks a blood supply and receives nutrition from the joint fluid. The meniscus has an unlimited blood supply. Without a blood supply and because of their relatively less active cellular makeup, the cartilage and meniscus do not maintain themselves. The cartilage and meniscus are extremely durable, but in time with “wear and tear” or following injury, they break down, fail, and lead to meniscus tears, cartilage damage, and eventually symptomatic (pain, stiffness, swelling) arthritis (failure of this protective joint surface).
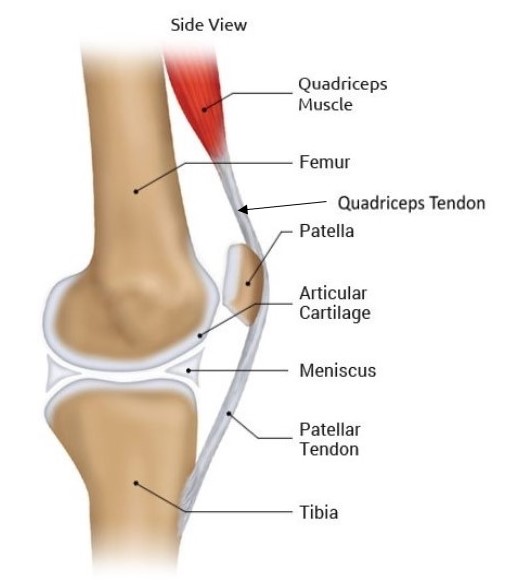 Tendons and Muscles
Tendons and Muscles
Tendons also help provide knee joint stability and movement. They act like strong cables connecting your muscles to your bones. These muscle-tendon units cross joints to compress, hold and move joints in specific directions. Like other parts of your knee, they are susceptible to injury and overuse. The two knee tendons most commonly injured are the quadriceps and patellar tendons.
Anterior Cruciate Ligament
The Anterior Cruciate Ligament (ACL) is the most well known of the knee ligaments because it is the one most often injured by athletes. When torn, the ACL does not heal and the knee can be unstable (shifts or gives way), especially during sports that require pivoting, changing direction (cutting), jumping, or landing. About one-half of the people who tear their ACL also tear their meniscus in their knee.
The ACL is one of a pair of cruciate ligaments in the human knee. The other is the Posterior Cruciate (PCL). The two ligaments also are called “cruciform” ligaments because they cross each other forming an “X”. The ACL is a ropelike structure composed of strong collagen fibrils that help maintain the normal relationship of the femur (thigh bone) and the tibia (leg bone) as the knee moves.
ACL Injuries & Conditions
ACL & Associated Meniscus Surgical Procedures
- Arthroscopic Anatomic ACL Reconstruction
- Arthroscopic Pediatric (Growth Plate Sparing) ACL Reconstruction (Developed by Dr. Chudik)
- Tibial Spine Avulsion Surgery for Pediatric Patients
- Anterolateral Ligament (ALL) Reconstruction
- Tunnelless Anatomic Arthroscopic Anterior Cruciate Ligament Reconstructive Surgery
- Tunnelless Posterior Cruciate Ligament (PCL) Reconstruction
- Medial Patellofemoral Ligament (MPFL) Tunnelless Reconstruction
- Arthroscopic Meniscus Repair
- Arthroscopic Meniscus Transplant
- Arthroscopic Partial Meniscectomy
- Arthroscopic Meniscus Repair vs. Meniscectomy
About Dr. Chudik

- Curriculum Vitae (CV)
- Video
- Website: stevenchudikmd.com
- Schedule an appointment online
- Email: contactus@chudikmd.com
- Phone: 630-324-0402
Innovations
Through his research, Dr. Chudik investigates and pioneers advanced and novel arthroscopic procedures, instruments and implants that change patients’ lives because of better outcomes. His efforts continue to yield scores of patents that will positively affect orthopaedic surgical techniques worldwide.

Novel Procedures
- Arthroscopic Pediatric (Growth Plate Sparing) ACL Reconstruction (Developed by Dr. Chudik)
- Arthroscopic ACL revision reconstruction, single stage
- Tunnelless Anatomic Arthroscopic Anterior Cruciate Ligament Reconstructive Surgery
- Medial Patellofemoral Ligament (MPFL) tunnelless reconstruction
- Tunnelless Posterior Cruciate Ligament (PCL) reconstruction
- Return to sport training program
- Return to sport testing
US Patents and Patent Applications
Dr. Steven Chudik continually innovates to create new technology surgical techniques and improve patient care. He also collaborates worldwide with other leaders in the orthopaedic technology industry. Surgeries provide Dr. Chudik with an endless source of ideas to create new, safer, less invasive, and more effective surgical procedures, surgical instruments, and implants. Several of his patents are the direct result of these pioneering endeavors.
- Method of Minimally Invasive Shoulder Replacement Surgery, U.S. Patent No. 9,445,910, filed September 11, 2006
- Humeral Implant for Minimally Invasive Shoulder Replacement Surgery. Patent application serial number 11/529,185 case II, filed September 25, 2006
- Glenoid Implant for Minimally Invasive Shoulder Replacement Surgery, U.S. Patent No. 9,974,658, filed September 25, 2006
- Humeral Implant for Minimally Invasive Shoulder Replacement Surgery, Serial No.11/525,629, filed September 25, 2006, application published as U.S. Patent App. Pub. 2007/0016305 (A)
- Guide for Shoulder Surgery, U.S. Patent No. 9,968,459, filed September 29, 2006
- Suture Pin Device. Patent application serial number 11/529,2006, case XV, filed September 29, 2006
- Suture Pin Device, Serial No. 11/529,185, filed September 29, 2006, application published as U.S. Patent App. Pub. 2007/0027477 (A)
- Method of Arthroscopic or Open Rotator Cuff Repair Using An Insertional Guide For Delivering a Suture Pin, U.S. Patent No. 8,540,737, filed October 24, 2006
- Acromioclavicular Joint Repair System, U.S. Patent No. 9,387,011, filed February 2, 2007
- Resurfacing Implant for a Humeral Head, Serial No. 13/068,309, filed May 9, 2011, application published as U.S. Patent App. Pub. 2012/0041563 (A)
- Universal Anterior Cruciate Ligament Repair and Reconstruction System(Cannulated Scalpel), U.S. Patent No. 10,034,674, filed February 2, 2007
- Resurfacing Implant for a Humeral Head. Patent application serial number 13/068,309 case II (A), filed May 9, 2011
- Method of Arthroscopic or Open Rotator Cuff Repair Using an Insertional Guide for Delivering a Suture Pin. U.S. Patent Number 8,540,737 B2, issued September 24, 2013
- Cortical Loop Fixation System for Ligament and Tendon Reconstruction, Serial No. 13/998,567, filed November 12, 2013, application published as U.S. Patent App. Pub. 2015/0134060 (A)
- Acromioclavicular Joint Repair System. U.S. Patent Number 9,387,011 B2, issued July 12, 2016
- Method of Minimally Invasive Shoulder Replacement Surgery. U.S. Patent Number 9,445,910 B2, issued September 20, 2016
- Guide for Shoulder Surgery. U.S. Patent Number 9,968,459 B2, issued May 15, 2018
- Glenoid Implant for Minimally Invasive Shoulder Replacement Surgery. U.S. Patent Number 9,974,658 B2, issued May 22, 2018
- Glenoid Implant with Replaceable Articulating Portion, U.S. Patent No. 11,406,505, filed August 20, 2019, issued August 9, 2022
- Cortical Loop Fixation Method for Ligament and Bone Reconstruction, Serial No. 15/731,719, filed July 24, 2017, application published as U.S. Patent App. Pub. 2019/0021845 (Pending)
- Humeral Implant and Method, Serial No. 17/532,714, filed November 22, 2021 (Pending), published as U.S. Patent App. Pub. US 2023/0157832
- Humeral Implant with Cannulation and Method, Serial No. 18/211,396, filed June 19, 2023 (Pending)
- Glenoid implant with Portal and Method, filed July 2023 (Pending)
Research
An inquisitive nature was the impetus for Dr. Steven Chudik’s career as a fellowship-trained and board-certified orthopaedic surgeon, sports medicine physician, and arthroscopic pioneer for treating ACL injuries. It also led him to design and patent special arthroscopic surgical procedures and instruments and create the Orthopaedic Surgery and Sports Medicine Teaching and Research Foundation (OTRF). Through OTRF, Dr. Chudik conducts unbiased orthopaedic research, provides up-to-date medical information to help prevent sports injuries, and shares his expertise and passion for mentoring medical students in an honors research program. He also serves as a consultant and advisor for other orthopaedic companies and industry.
Areas of Knee Research & Development